Early in the COVID-19 pandemic, as Americans grappled with the disruptions surrounding the first quarantine period, some diabetic foot specialists sounded a warning about an impending spike in limb loss.
“The outpatient management of people with diabetes and its complications is facing a huge challenge,” wrote Laura Shin of the University of Southern California’s Keck School of Medicine, in a paper she and three coauthors submitted last May. “Routine face-to-face clinics have been canceled in many countries, and the ability to order even basic tests has been severely restricted…. There is the potential for a tsunami of problems, resulting in major surgery, amputation, and mortality, to occur in the months and even years after the full lockdown finishes.”
Nearly a year later, the pandemic’s impact on diabetes-related limb loss is starting to come into focus—and the picture isn’t pretty. Multiple investigations have shown sharp increases in diabetes-related amputations since the pandemic began, as individuals either are unable or reluctant to access necessary care.
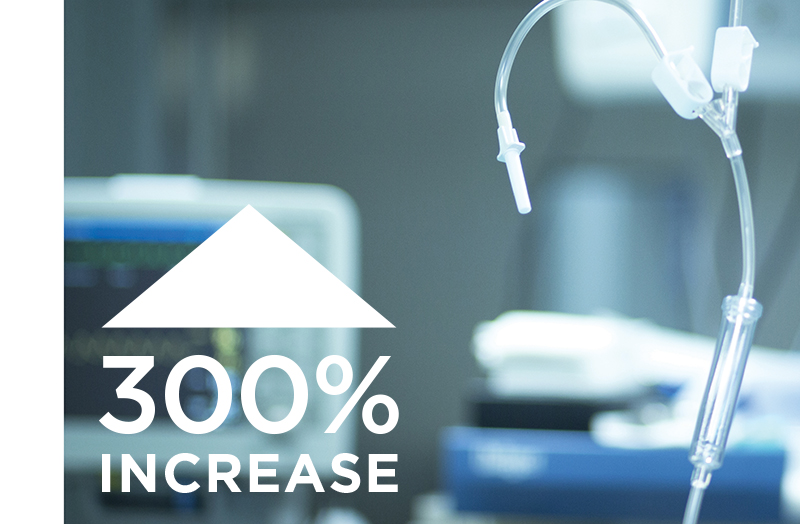
According to one study published online by the Journal of the American Podiatric Medicine Association (JAPMA), amputations at an Ohio trauma center increased nearly elevenfold after the pandemic took hold. Similar data that appeared in the Journal of Vascular Surgery showed a 300 percent increase in the rate of leg amputations in patients with diabetes at the University of California, San Francisco (UCSF). European researchers documented parallel trends in Italy and the Netherlands.
“It is likely that patients’ reluctance and fear to seek medical care during this period created complications that resulted in these catastrophic results,” wrote the editors of JAPMA, describing the spate of diabetes-related amputations as “a pandemic within a pandemic.”
“The recent acute increase in major amputations we have witnessed is a concerning trend that requires a strategic response from each practice, health system, and the public health sector,” wrote the authors of the UCSF study. “As our society and healthcare system adapt to the new changes required in the COVID-19 era, it is critical that we give special attention to the many vulnerable subsets of the vascular surgery population. Further study is needed to understand the underlying causes and the most effective methods to mitigate the negative outcomes now and prevent them in the future.”