Studies Show More Sprawl Associated with Higher Incidence of Poor Health Outcomes
Posted June 24, 2014
People who live in neighborhoods that are conducive to walking experienced a substantially lower rate of obesity, overweight, and diabetes than those who lived in more auto-dependent neighborhoods, according to a pair of studies presented at the American Diabetes Association’s 74th Scientific Sessions.
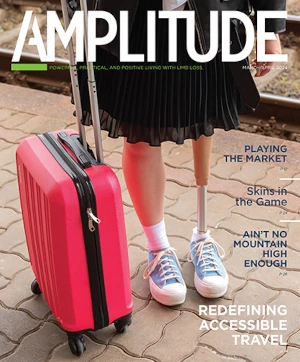
Since people with diabetes are at increased risk for serious health complications including vision loss; heart disease; stroke; kidney failure; tooth loss; amputation of toes, feet, and legs; and premature death, lowering the rate of the disease can also help prevent these negative health problems associated with it. Moreover, many amputees have an increased risk for diabetes, partly due to a lack of physical activity such as walking.
Researchers in Canada compared adults living in the most and least “walkable” metropolitan areas in southern Ontario and found a lower risk of developing diabetes over a 10-year period for those who lived in neighborhoods with less sprawl, more interconnectivity among streets, and more local stores and services within walking distance, among other measures used to determine a neighborhood’s “walkability.” The researchers controlled for variables, such as health at baseline, to rule out the probability that healthier people were choosing more walkable neighborhoods to begin with. A second study that compared neighborhoods, not individuals, found that the most walkable neighborhoods had the lowest incidence of obesity, overweight, and diabetes.
“How we build our cities matters in terms of our overall health,” said lead researcher Gillian Booth, MD, endocrinologist and research scientist at St. Michael’s Hospital and the Institute for Clinical Evaluative Sciences (ICES) in Toronto. “This is one piece of a puzzle that we can potentially do something about. As a society, we have engineered physical activity out of our lives. Every opportunity to walk, to get outside, to go to the corner store, or walk our children to school can have a big impact on our risk for diabetes and becoming overweight.”
Marisa Creatore, MSc, epidemiologist with the Centre for Research on Inner City Health at St. Michael’s Hospital, Toronto, added that the studies revealed the degree to which “your environment can influence your decisions about physical activity. When you live in a neighborhood designed to encourage people to be more active, you are in fact more likely to be more active.”
Specifically, the studies found that people living in neighborhoods with greater walkability saw on average a 13 percent lower development of diabetes incidence over 10 years than those that were less walkable. However, walkability was only protective in those who were younger and middle aged; those who were age 65 or older saw no benefit from living in a walkable neighborhood.
Diabetes was lowest in the most walkable neighborhoods, where incidence fell 7 percent over 10 years, whereas neighborhoods rated least walkable saw a 6 percent rise in diabetes over the same time period. Overweight and obesity, as well, was lowest in the most walkable neighborhoods and fell by 9 percent over 10 years, whereas it rose 13 percent in neighborhoods with the least walkability during that time.
The researchers also noted that people who lived in the most walkable neighborhoods were three times more likely to walk or bicycle and half as likely to drive as a means of transportation.
Solving the obesity pandemic, concluded Booth, “will require both policy changes as well as individual strategies. We have to take a more population-based approach to the problem, given the environment we live in.”