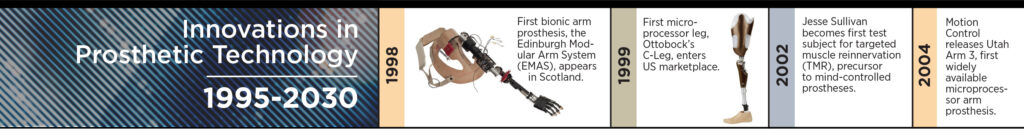
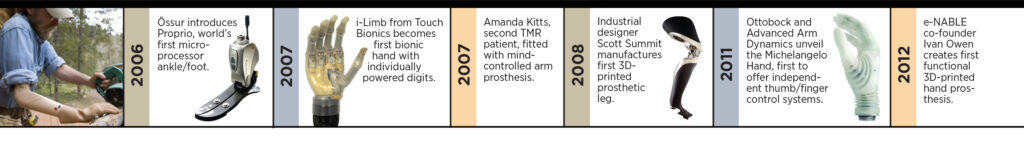
Big Breakthroughs in Prosthetic Technology Are Near at Hand

Consider how entertainment technology has changed over the last ten years.
If you wanted your favorite songs on demand back in 2011, you had to assemble the tunes yourself and burn them onto a CD. To binge-watch a TV series, you had to wait for the boxed-set release years after broadcast. Podcasts and YouTube did exist, but the pickings were painfully slim. And to see the latest Marvel Universe blockbuster, you either bought a ticket or waited months for the Netflix release.
Today you can download all that content on demand to a single, affordable device that fits in your hand and acts on voice commands. The clunky old mechanisms have been supplanted by an integrated delivery system that’s flexible, intuitive, and on-the-nose responsive.
Ten years from now, perhaps we’ll be looking back on a similar evolution in prosthetic technology. As advanced as today’s devices are, they’re prohibitively expensive for many amputees and often have a steep learning curve. But there’s a new generation of prostheses on the horizon that promise greater affordability and ease of use, with the potential to plug into our lives as seamlessly as a smartphone.
A MIND OF THEIR OWN
Prosthetic devices have been getting whip-smart throughout this century. But now the technology is verging beyond intelligence toward something more akin to awareness. Next-gen machines will not only improve amputees’ function but also restore feeling, achieving the type of mind-body integration that previously existed only in sci-fi movies and video games. Here’s a quick peek at what might be just around the bend.
Devices That Think

Utah Robotics Center
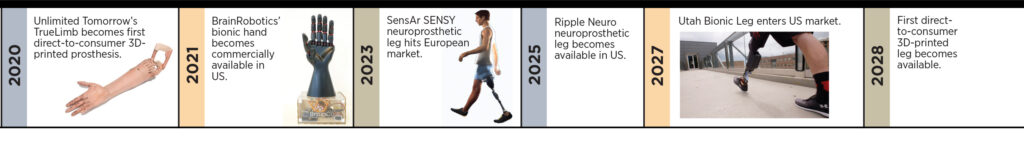
“I haven’t played a computer game in six years,” below-elbow amputee Carey Duval told the Washington Post in December 2020. That was before he started working with BrainRobotics’ futuristic myoelectric hand, which uses a machine-learning algorithm to translate muscle signals into precise movement. The device’s range of gestures and degree of control are said to be off the charts—it allowed Duval to deftly manipulate a mouse and keyboard. Another beta tester played piano while wearing the hand.
Time magazine named the BrainRobotics prosthesis one of the top inventions of 2019, and it took Top Tech honors at the 2020 Consumer Electronics Show. The hand is under FDA review, with approval expected in 2021. When it does hit the market, the BrainRobotics hand is expected to cost a relatively affordable $10,000 to $15,000.
Lower-limb amputees, despair not: The Utah Bionic Leg achieves similarly lifelike results with a different approach. Instead of taking its cues from muscle impulses, this supersmart prosthesis essentially reads your mind. By continuously monitoring its trajectory in relation to your body and the ground, the leg anticipates your movements to produce a smooth, effortless gait that feels in sync, rather than lagging a split-second behind.
Developed by Tomasso Lenzi in the Utah Robotics Center, the project recently received nearly $3 million in new funding from the National Science Foundation and the National Institutes of Health (NIH). It’s still a few years away from commercial release, but slightly ahead of a similar project that’s underway at North Carolina State. May the smartest leg win!
Devices That Feel

Smart prosthetics excel at receiving and acting on signals from the brain. Neuroprosthetics open a second channel of communication: They not only hear the brain’s commands, they also send information back.
Here’s how it works. The prosthesis is equipped with electronic sensors that continuously transmit wireless signals about position, contact, force, and other variables. Those signals are received by electrodes that are implanted within the amputee’s residual limb and wrapped around the major nerve (also called the peripheral nerve). From there, the feedback gets relayed to the brain via normal neural pathways, enabling the user to “feel” through the prosthesis.
That’s exactly the sensation reported by early testers of the SENSY, a neuroprosthetic leg that’s being developed collaboratively by Össur and an Italian company called SensArs Neuroprosthetics. The device cleared preliminary trials last year, with participants reporting better balance, surer footing, less fatigue, and a reduction in phantom pain. A full-scale clinical study is in progress, with results expected next year.
Clinical results are also expected in 2022 from Utah-based Ripple Neuro, which is funneling $2 million in NIH funding into a neuroprosthetic leg that uses the same approach as the SENSY. The company is also partnering with the University of Utah to apply this concept to endow neuroprosthetic hands with the sense of touch.
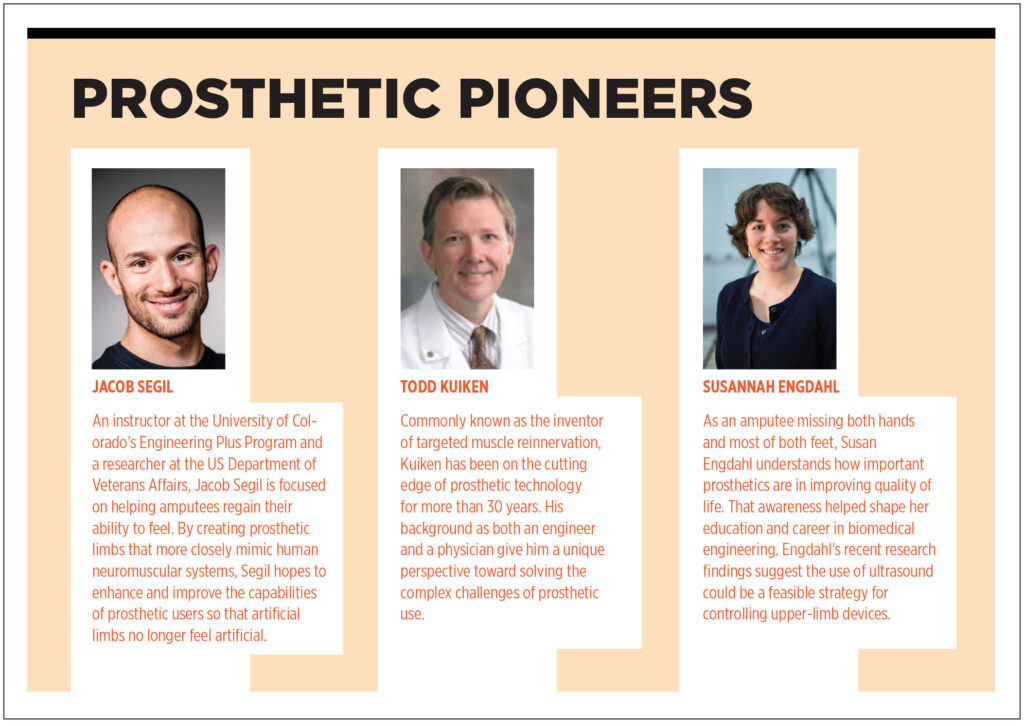
DISRUPTORS AND DISPENSERS
Fewer than half of US amputees today have access to a prosthesis. Worldwide, that figure is below 10 percent. With so many people left out of the revolution in advanced prosthetic technology, the greatest impact on the future of living with limb loss may come from a parallel revolution that’s focused on making devices more affordable and more widely available. Meet some of this movement’s key leaders.
Factory Direct
Despite all the buzz Easton LaChappelle has generated to date, the 25-year-old inventor is just getting started. Since developing his bionic arm as a teenager a few years ago, he has drawn approval from then-President Barack Obama, made Forbes magazine’s 30 under 30 list of rising entrepreneurs, and partnered with Microsoft and the US Department of Defense. Last year his three-year-old company, Unlimited Tomorrow, appeared on Inc. magazine’s “Best in Business” list of the nation’s most innovative firms.
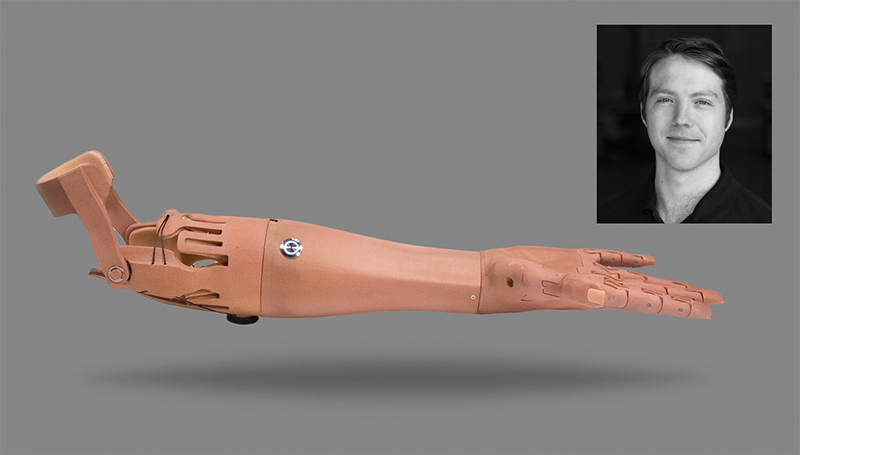
That’s a lot of acclaim for a startup whose first product, a 3D-printed arm prosthesis called the TrueLimb, was just released nine months ago. But Unlimited Tomorrow’s core innovation lies not with its product but with its process. The company is marketing the TrueLimb using a direct-to-consumer approach that completely bypasses insurers and prosthetic caregivers. You scan your own residual limb, using equipment the company ships to your home. The fitting takes place via a remote consultation with one of TrueLimb’s engineers, and you have the option to pay on a budget-friendly installment plan.
These efficiencies enable Unlimited Tomorrow to price the TrueLimb far below what name-brand competitors charge. They also give consumers a feeling of empowerment. Many prosthetists understandably feel differently: They’re concerned that Unlimited Tomorrow purports to address a medical need with a device that’s not backed by any input from clinical experts. “There will always need to be a trained prosthetic professional available to fit and optimize this new technology,” Gerald Stark, a certified prosthetist and senior clinical specialist at Ottobock, told The O&P EDGE.
LaChappelle points out that he’s consulted with medical/clinical experts at every stage of the TrueLimb’s development. “We have a robust clinical advisory board and clinicians on staff,” he says. And some prosthetists see LaChapelle’s model as an opportunity to expand their own business and help more amputees. “3D printing is only going to get better, cheaper, and more pervasive in its O&P applications,” writes certified prosthetist Jeremaiah Uronis. “The only course of action is for us to become more active members in the applied use of 3D printing in O&P.”
No Insurance? No Problem.
When he lost his right arm below the elbow in 2017, Nate Munro saw the US healthcare system through new eyes. “I realized I was living in a first-world country for people with insurance,” he told an interviewer last year, “but a developing country for those without insurance.”

Unable to meet his prosthetic needs through normal channels, Munro—a veteran engineering consultant—joined the limb-loss community’s global “do-acracy”: e-NABLE. Founded in 2012 by a self-taught 3D-printing hobbyist, e-NABLE has grown into a worldwide collective of do-it-yourself prosthetic designers who share ideas, eschew profits, and offer solutions to amputees who are priced out of the conventional market.
“We want to make sure we only offer simple and inexpensive solutions when they really are solutions,” e-NABLE co-founder John Schull told The O&P EDGE in 2015. A former professor at the Rochester Institute of Technology, Schull thinks grassroots efforts like his should complement, rather than compete with, the O&P industry. He tries to build partnerships that help e-NABLE’s products gain more clinical acceptance among prosthetists.
Munro’s work offers a step in that direction. He has spent the last couple of years developing the No-Insurance Optimized Prosthetic (NOIP) system, a five-stage modular arm that has raised technical standards in the e-NABLE catalog to a new level. “It’s kind of funny that it was easier to create a whole line of prosthetics than to work within the broken healthcare system dominated by the insurance industry,” Munro says. “This obstacle became the inspiration for developing a disruptive technology to throw into the market—a protest in some ways, but also a solution.”
One Size Fits All
As a graduate student at Northwestern University and the Massachusetts Institute of Technology, Elliott Rouse was vexed by the lack of coordination among researchers in the field of bionic prosthetics. Every lab used its own hardware system, imposing high start-up costs and creating a jumble of systems that kept researchers from sharing knowledge and building on each other’s findings.

Department of Mechanical Engineering
So, taking a page from e-NABLE’s playbook, Rouse developed a basic blueprint and shared it freely. Published last October in the journal Nature Biomedical Engineering, the Open Source Leg (OSL) features state-of-the-art hardware, artificially intelligent control systems, and baseline performance data gathered by the Shirley Ryan Ability Lab. The OSL gives future researchers a new, standardized foundation on which to build, while opening the door to novel opportunities for collaboration with doctors, physical therapists, athletic trainers, and other experts.
“It will enable investigators to efficiently solve challenges associated with controlling bionic legs across a range of activities in the lab and out in the community,” says Rouse, “and enable new investigators from related fields to develop innovative control strategies.”
“The OSL effectively lowers the barriers to entry for researchers,” adds Levi Hargrove, the Shirley Ryan Ability Lab’s director of biomedicine. “It’s a plug-and-play system that allows scientists to avoid research and development costs in the millions of dollars and immediately begin testing on prosthetics.”
In essence, the OSL will do for researchers what e-NABLE is doing for amputees—reduce costs and broaden access in the name of progress. “This represents the future of research,” says Rouse.