When vascular conditions such as diabetes or peripheral artery disease (PAD) reach the limb-threatening stage, the best shot to avoid amputation is generally revascularization. But patients often can’t get the procedure if they don’t have adequate insurance, resulting in avoidable limb loss. A new study shows how easily this problem can be solved: Insuring more people leads to a drastic reduction in vascular-related amputations.
Published this summer in a special edition of The American Surgeon, the study was authored by researchers from Howard University Medical School and the University of Alabama at Birmingham. They examined revascularization rates in Maryland (adjacent to Howard’s location in Washington DC) among patients with critical limb-threatening ischemia (CLTI), which is closely associated with diabetes and peripheral artery disease. While revascularization can’t prevent amputation for every CLTI patient, it’s most effective when CLTI is detected early and managed carefully. But that’s far less likely to happen for uninsured and underinsured individuals.
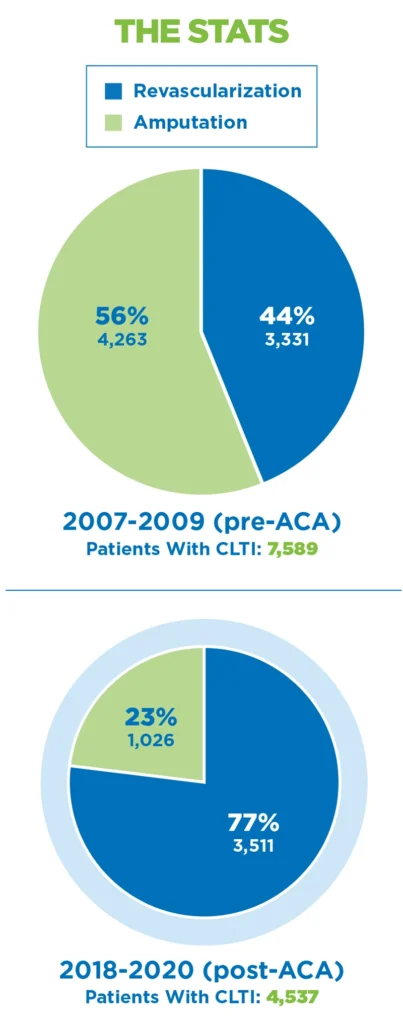
The American Surgeon paper compared Maryland’s amputation and revascularization rates at two segments in time: before and after the implementation of the Affordable Care Act (ACA), which helped tens of millions of Americans obtain insurance. Maryland’s uninsured population dropped from about 600,000 residents in the last year pre-ACA to roughly 350,000 in 2022, meaning that roughly 250,000 low- and middle-income Marylanders gained insurance via the ACA.
The accompanying infographic shows how the broadening of insurance affected limb loss in Maryland: Amputation rates dropped from 56 percent to 23 percent after ACA implementation, while revascularization rates soared from 44 to 77 percent. Just as significant, total CLTI cases dropped by 40 percent between the pre- and post-ACA periods. Presumably, broader insurance coverage enabled more people to obtain basic, routine care, which in turn led to better preventive care for people with diabetes and PAD and a sharp reduction in the number of cases that advanced to the CLTI stage.
The improved outcomes for CLTI patients “may stem from the ACA’s role in enhancing access to specialized care and advanced treatment options,” the authors wrote. “It could also imply that with broader insurance coverage, patients are now presenting earlier in their disease stage, where they are more likely to be candidates for revascularization.”
The Howard researchers also found that long-range outcomes for CLTI patients improved in the ACA era. Average length of hospitalization was shorter for patients in both the revascularization and amputation cohorts. Even more encouraging, mortality rates dropped by 30 percent for patients undergoing revascularization and by 55 percent for patients who experience amputation.
This study is consistent with a number of prior investigations that examine the ACA’s effect on amputation rates. One, published in 2020 by the American Diabetes Association, found that amputation rates in the post-ACA period dropped sharply among minority patients with diabetic foot ulcers. Another, published in the Annals of Vascular Surgery in 2018, found that patients with vascular disease in Arkansas enjoyed a 26 percent reduction in the odds of amputation post-ACA. And a 2022 research paper in JAMA Network Open found that amputation rates decreased among minority patients with diabetes.
The full paper is available online at journals.sagepub.com/home/asu.




