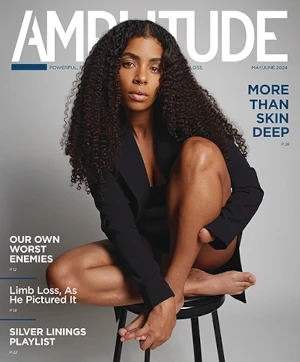
by Larry Borowsky

Courtesy Aristotle Domingo.
As attendees walked the exhibit floor at the American Orthotic and Prosthetic Association’s annual conference last fall, some might have wondered if they’d come to the wrong hotel by mistake. Booth after booth greeted visitors with displays about 3D printing rather than prosthetics. Plenty of 3D-printed sockets and limbs were available for inspection, of course. But there were also trays of resin and filament and powder, computer screens with demos of modeling software, and stacks of brochures and white papers about digital prosthetics’ cost, comfort, and strength. For the first time in its history, the AOPA conference offered a Digital Care education track featuring half a dozen sessions about 3D printing. And anyone who wanted an up-close-and-personal peek at the technology could attend a two-hour Digital Care Showcase, also making its debut at the 2022 conference.
The 3D-printing revolution has been approaching for so long that most of us in the limb-loss community feel pretty well informed on the subject. But we’ve generally glimpsed this technology as an indistinct blip on the horizon. Now that the ship is actually sailing into port, people are realizing how much we don’t know about 3D-printed prosthetics, and how the hazy outline we’re familiar with leaves a lot of blanks to fill in.
It’s also becoming clear that much of our attention has been focused on devices that don’t fully reflect the technology’s potential impact on amputees’ lives. We see the daring aesthetics that can be achieved via 3D printers, and we read about the uplifting humanitarian projects. Occasionally we hear about possible improvements to cost, comfort, and usability. What’s generally left out is the most exciting part—the paradigm shift in how prosthetic devices are produced, distributed, and paid for.
In a nutshell, 3D printing equips the industry to churn out custom devices—designed and built to fit individual bodies—at vastly greater speed and volume than traditional production methods. “It’s a new platform,” says prosthetist Chris Hutchison, co-founder and chief technology officer of ProsFit, one of 3D-printed prosthetics’ pioneering firms. “It’s much more flexible and mobile [than the current model], and it not only provides better care for amputees but also brings new opportunities for professionals in prosthetics, so they become more entrepreneurial and more hands-on.”
That explains why 3D printing had such a strong presence at the AOPA conference. It’s already starting to change the way prosthetists do business, and that has obvious implications for the amputees they serve. Change can be scary and confusing, and it’s inherently prone to misunderstandings and mistaken impressions. So as 3D printing cruises into the harbor, we thought we’d challenge a few myths about the technology.
MYTH #1
3D-printed prosthetics are cheap, inferior knockoffs of conventionally produced devices.
This misperception arises in part from the media’s fascination with brainy teens who design and 3D-print fully functioning bionic limbs. The most visible US manufacturer of 3D-printed prosthetics, Unlimited Tomorrow, has its roots in that narrative: Company founder Easton LaChappelle first gained notoriety a decade ago as a science-fair whiz kid with a homemade bionic hand.
But LaChappelle will be the first to tell you that his company’s TrueLimb is no science-fair project. It’s an elaborately engineered machine that’s fabricated on industrial-grade 3D printers using state-of-the-art composites, high-level sensors, and advanced algorithms. Time will tell whether the TrueLimb endures as a prosthetic solution, but it’s already established as a credible competitor in its market.
A corresponding staple of mass media coverage involves the widespread disbursement of 3D-printed limbs in developing regions at little or no cost. These devices improve the lives of thousands of amputees who would otherwise lack access to even a basic prosthesis. But because they’re virtually given away, they feed the belief that 3D printers can only manufacture rudimentary, low-cost gadgets.
“It’s a spectrum,” says Hutchison. “It runs from middle-schoolers 3D-printing limbs out of melted bottle tops, all the way to the type of manufacturing we’re doing, which is literally using the same technology that goes into building rockets.”
Founded in 2016, ProsFit (which is based in Bulgaria) provides a seamless end-to-end solution for 3D-printed sockets, saving clinicians the trouble and expense of buying, mastering, and maintaining all the underlying technology. Prosthetists scan patients’ limbs at the point of care and build a preliminary model using a cloud-based software platform. They release the files to ProsFit’s engineers, who refine the model and vet it for regulatory compliance and quality assurance. The final output files are transmitted to a commercial 3D-printing facility (ProsFit has affiliates around the world), where the socket is manufactured. Total turnaround time, from scan to delivery, is usually less than two weeks. (See below for a step-by-step summary of the production sequence.)
“This is very serious, high-end manufacturing,” Hutchison says. “We work with BASF, one of the largest materials companies in the world, and SGL Carbon, one of the largest carbon manufacturers in the world. We’re doing the same type of thing that’s being done in the aerospace, defense, and automotive industries.” He adds that ProsFit’s sockets meet the European Union’s rigorous specs for medical-device designation. They also have achieved the same quality certification (ISO 10328) as conventionally produced devices. “We have to be extremely rigorous. All our research and testing and procedures are reviewed and audited very thoroughly by the government agencies.”
Early generations of 3D-printed arms and sockets were largely fabricated from materials of a similar grade to the thermoplastics that go into conventional check sockets. They were therefore prone to weakness, cracking, and outright failure. But today’s leading-edge devices use sophisticated powders and resins that compare favorably with carbon fiber in terms of strength and structural integrity.
That came as a pleasant surprise to actor and athlete Aristotle Domingo, a Canadian bilateral amputee who’d formed a dim view of 3D-printed sockets after trying some in the late 2010s. “The stuff they printed out was completely useless to me,” he says. When he grudgingly agreed to try a pair of ProsFit sockets in 2020, they greatly exceeded his low expectations. “I thought it was going to be garbage,” he laughs. “But their socket fit like a glove right away. It relieved all the pressure points on my [right] distal end, so I got rid of all my sores there. On my left, my fib head isn’t rubbing at all. We didn’t need to add any padding or cushioning. It just fit that way.”
“It felt like a natural extension of my body, and the fit was perfect,” adds martial artist Rustin Hughes, who’s also been wearing a 3D-printed socket since 2020. “The sockets are built off a scan of your leg, so it’s way more precise than the conventional method. And the 3D[-printed] socket is crazy light. Ounces mean a lot in above-the-knee amputees. That’s something I noticed immediately.”
Domingo’s opinion of 3D-printed sockets has done a 180. “I’ve been wearing my ProsFits since the day I got them,” he says. “It’s coming up on three years. I wouldn’t switch back to my old socket system.”
MYTH #2
3D-printed prosthetics are still untested.
This idea springs in part from the same source as Myth #1: Popular media tend to overrepresent the DIY end of the 3D-printing spectrum, while underrepresenting the evidence-supported scientific/industrial end. As a result, most people don’t realize how much data underpins the current generation of 3D-printed prosthetics.
That body of evidence is at least 18 years old and probably older. The earliest peer-reviewed study of 3D-printed prosthetics we could find, titled “A Preliminary Investigation Into the Development of 3-D Printing of Prosthetic Sockets,” appeared in 2005 in the Journal of Rehabilitation Research and Development. “Under normal circumstances, printed components are weak and relatively fragile,” the authors of that paper wrote. However, “with careful resin selection, the mechanical strength of a 3DP component has been shown to increase to an extent that would make it suitable for use in prosthetic devices.”

Hundreds of academic investigations have ensued, and private-sector companies have invested untold millions in proprietary R&D. Engineers have refined every step of the production sequence for 3D-printed prosthetics, from raw materials to design, manufacturing, and waste recovery. On the clinical side, healthcare researchers have measured patient outcomes such as mobility, dexterity, pain, and overall fitness.
“Our clinic has 100 patients who are living proof that this technology works,” says certified prosthetist Joe Johnson, owner of Quorum Prosthetics. “We know it works, and we have the data to back it up.”
One of just a handful of US prosthetic clinics with in-house 3D-printing capacity, Quorum has partnered with the Department of Veterans Affairs and two Colorado universities to gather outcomes data about Quorum’s 3D-printed socket (called the Quatro). One study showed that the Quatro improved amputees’ gait symmetry and reduced their overall walking effort. Another compared pressure distribution in the Quatro to that of a conventional socket, yielding quantitative evidence that affirms patients’ subjective reports of socket comfort.
As 3D-printed limbs inch closer to commercial viability, research activity is accelerating. Limbitless Solutions, a Florida-based nonprofit startup, is conducting an ongoing series of clinical trials to gather data about its 3D-printed bionic arm. Quorum is launching a new study with the University of Colorado to test whether 3D-printed sockets can improve proprioception. ProsFit recently published the results of a year-long study involving mobile, in-home scanning and fitting of their sockets. In 2022 alone, nearly 100 new papers about 3D-printed prosthetics appeared in peer-reviewed medical, scientific, and technical journals.
One of those 2022 papers, a systemic literature review that aggregated data from multiple studies, concluded that “preliminary experimental clinical data suggests that [3D-printed sockets] may be safe and effective for daily use.” That’s not to say the efficacy of 3D-printed models is definitively proven. But you can rest assured that the technology has been, and will continue to be, evaluated for its safety, performance, and health impacts.
MYTH #3
3D printing will drive prosthetists out of business.
Amputees tend to push back reflexively on anything that threatens to alter their relationship with their prosthetist. And few are enthusiastic about having their limb care transferred from an attentive, hands-on clinical team to a crew of Geek Squad techies—or, worse, a bot from Hewlett-Packard’s help desk.
But that’s not what 3D printing will do, says Domingo. When he went through the design process for his ProsFit sockets, he collaborated with his prosthetist (a Toronto-based ProsFit affiliate) as closely as he would have for a conventional plaster-and-lamination fitting.
“She scanned my limb,” he says, “and then we looked at the image together. When we started building the model, I threw a whole bunch of things at her: ‘Let’s put some padding here and a shim there. This feature is hitting the bottom of my leg, and that one’s pushing up on my knee. Must have this, cannot have that.’ It was all the same information you would convey to an old-school prosthetic tech.”
“What we’ve seen is that being involved in the design process—actually being there during the CAD/CAM process—has meant that people can give more detailed feedback than ever,” notes Hutchison. “They feel more involved, and they’re psychologically more prepared for the final result because they have buy-in. They literally helped build it.”
Amputees aren’t the only ones who are anxious about how 3D printing might upend patient-prosthetist dynamics. Many clinicians regard this new technology the same way John Henry viewed the steam-powered drill—as a senseless brute with plenty of muscle but no brains or heart. It’s a natural reaction for practitioners who take pride in their craft and are sensitive to patients’ needs. But as the AOPA conference suggests, the industry as a whole is beginning to view 3D printing as a help, not a hindrance, to their professional mission.
“Two years ago, when I was looking into this, there were definitely still people who were bad-mouthing the whole idea,” says Johnson. “They were going out of their way to look for reasons why it wouldn’t work. But now it’s generally accepted that this is happening, and everyone’s got to get on the train.”
An amputee since the age of 15, Johnson has witnessed multiple stages of technological change. “I remember when silicone liners came out in the late 1980s,” he says. “There were people who said, ‘Silicone liners will never work. I don’t understand why you’d even bother, wool socks are just as good.’ And then carbon fiber feet came out, and it was the same thing: ‘Seattle Feet are the best, don’t bother walking on carbon fiber.’”
“Professionals tend to have a fear of the unknown,” says Hutchison. “And right now, fear of the unknown is greater than the fear of missing out. But people are starting to see that this is an incredible tool set that takes them far beyond what they were capable of achieving before. ”
ProsFit, which already has affiliate clinics throughout Europe, southeast Asia, and Africa, is planning to enter the US market in 2023, although Hutchison says “it’s more important for us to do it correctly than to do it quickly.” In the meantime, American consumers who are curious about 3D prosthetic devices have plenty of other options. Upper-limb amputees can purchase a TrueLimb or an Open Bionics Hero Arm. And many clinicians now offer 3D-printed sockets to leg amputees, though often on a limited basis. A very small number (Quorum and North Carolina-based EastPoint Prosthetics are two examples) have developed their own comprehensive, end-to-end 3D-printing capacity. Last year Protosthetics, a central fabricating facility based in North Dakota, launched an affiliate-based scan-design-print model that resembles ProsFit’s end-to-end solution. And dozens of clinics have dipped their toes in the water, performing routine production steps such as scanning (and, possibly, 3D modeling) in-house while outsourcing the more complex engineering and manufacturing operations.
Hutchison didn’t attend the AOPA conference, but he’s taken note of 3D-printing colonies at other O&P trade shows. “We’re seeing things at booths that look like things we built five years ago,” he laughs. “So that’s kind of comforting, because it means 3D printing is coming. And we think it will make the whole system more flexible so it’s better for amputees in receiving care.”
3D-Printed Prosthetic Devices: Step by Step
How will 3D printing change your visit to the O&P clinic? Here’s an abridged guide to the process of getting a 3D-printed prosthetic socket. Images courtesy ProsFit Technologies.
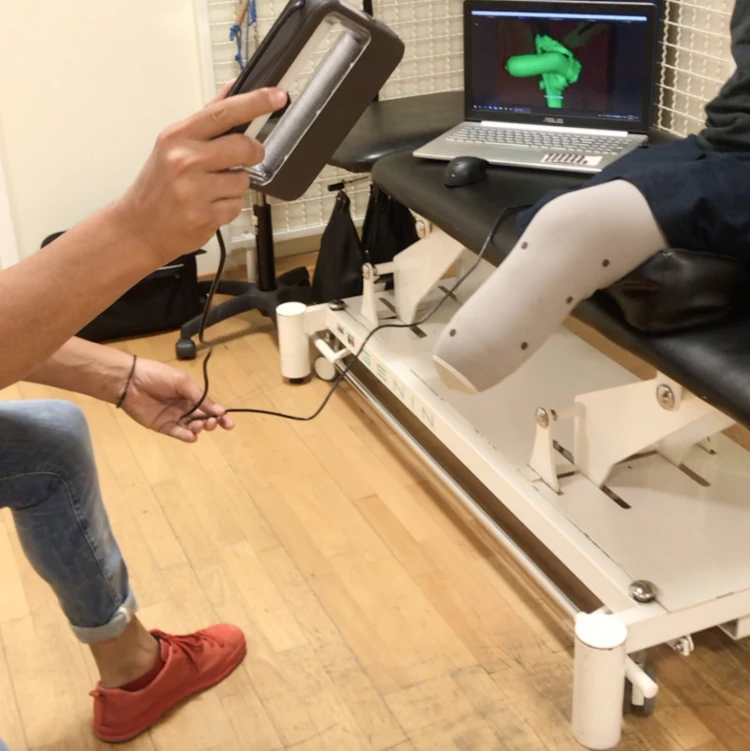
a basic 3D image. Elapsed time: a few minutes.
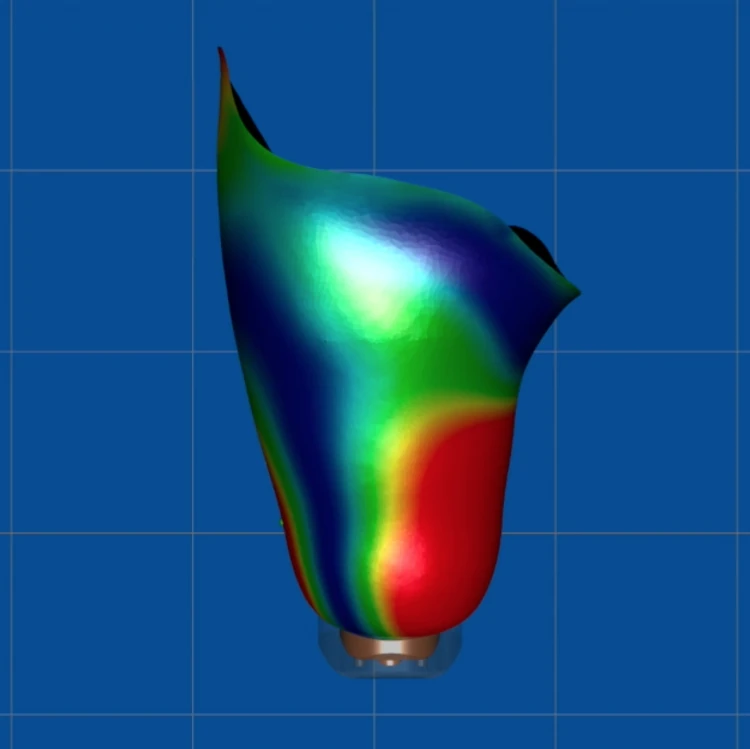
custom-designed 3D model. Elapsed time: 1 to 2 hours,

for manufacturing. Elapsed time: 2 to 5 business days.

final fitting. Total turnaround time: 1 to 2 weeks.