Researchers at Indiana University (IU) School of Medicine have found a way to charge up the fight against bacterial infections using electricity.
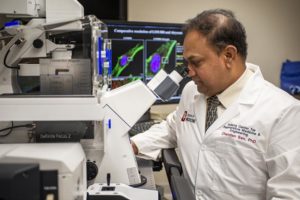
Work conducted by Chandan Sen, PhD, and Sashwati Roy, PhD, has led to the development of a dressing that uses an electric field to disrupt biofilm infection. Their findings were published in Annals of Surgery.
Bacterial biofilms are thin, slimy films of bacteria that form on some wounds, including burns or post-surgical infections, and after a medical device, such as a catheter, is placed in the body. These bacteria generate their own electricity, using electric fields to communicate and form the biofilm, which makes them more hostile and difficult to treat. The Centers for Disease Control and Prevention estimates 65 percent of all infections are caused by bacteria with this biofilm phenotype, while the National Institutes of Health estimates that number is closer to 80 percent.
Researchers at IU School of Medicine are the first to study the practice of using an electric field-based dressing to treat biofilms rather than antibiotics. They discovered that the dressing is not only successful in fighting the bacteria on its own, but improves the efficacy of other medications when used in combination. This discovery has the potential to create significant changes in the way physicians treat patients with bacterial infections that are resistant to antibiotics. The dressing can also help prevent new biofilm infections from forming in the future. The dressing electrochemically self-generates one volt of electricity upon contact with body fluids such as wound fluid or blood, which is not enough to hurt or electrocute the patient.
“This shows for the first time that bacterial biofilm can be disrupted by using an electroceutical dressing,” said Sen, director of the Indiana Center for Regenerative Medicine and Engineering and associate vice president of research for the IU School of Medicine Department of Surgery. “This has implications across surgery as biofilm presence can lead to many complications in successful surgical outcomes. Such textile may be considered for serving as hospital fabric—a major source of hospital-acquired infections.”
Marketing of the dressing for burn care was recently approved by the Food and Drug Administration. The team is now studying the device’s effectiveness in patients recovering from burns.
This article was adapted from information provided by IU.