In our November issue, we included a short list of takeaways from the 1st International Conference on Phantom Limb Pain (ICPLP), which took place last September in Mölndal, Sweden. Last week the full proceedings were published online, including full-length videos of every session, presentation, and panel discussion.
It’s a lot of material to plow through, and much of it is too speculative or theoretical to have any practical value at present. But one line of inquiry piqued our curiosity: a major clinical study of phantom motor execution (PME). It caught our attention because the research is being supervised by the esteemed Max Ortiz Catalán, founder of the Center for Bionics and Pain Research and a pioneer in the use of virtual reality and augmented reality to reduce PLP.
At the ICPLP, Catalán’s team gave a live demonstration of PME and presented data from the first-ever randomized controlled study of the treatment’s effectiveness. Here’s what we learned.
The theory behind phantom motor execution
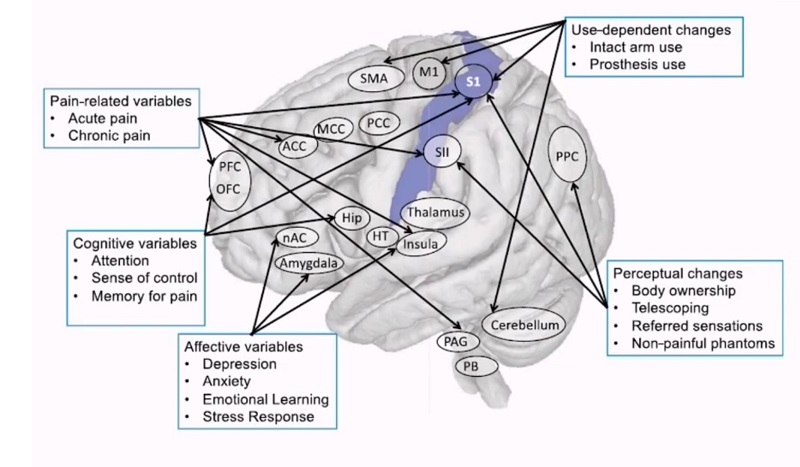
Phantom motor execution rests on the same premise as mirror therapy—ie, that PLP is rooted in disruption of the brain’s map of the body. Per this theory, the brain sector that’s assigned to the amputated part(s) of your body goes a little haywire, casting about to pick up a signal on a channel that has suddenly gone dark. Mirror therapy and similar approaches attempt to bring the mind’s spatial template back into harmony with the physical body.
Phantom motor execution achieves this realignment by having the patient manipulate their phantom limb in specific ways, while seeing the effects of the corresponding limb movements in augmented reality or virtual reality. Electrodes on the surface of the residual limb measure the neuromuscular activity involved in these maneuvers, and the patterns are fed into an algorithm. With practice, the phantom limb can become highly responsive to specific mental commands, as illustrated during the live demo at the ICPLP.
In that exercise (which you can watch here beginning at the 1:00:46 time stamp), a right below-elbow amputee uses phantom motor execution to open and close the (virtual) fist of his missing hand, rotate his forearm, and even flex his pinky finger. Later on, the subject twirls the cursor on a computer screen for a round of Breakout, an old Atari classic from the Stone Age of video gaming (watch this clip if you’re too young to recall Breakout, kiddies). He also operates a virtual joystick to drive a video-game car.
What does this type of activity have to do with reducing PLP? That’s the question Catalán and his crew are still trying to answer. They’ve conducted enough tests to establish that amputees who practice PME reliably experience a reduction in phantom limb pain. What’s still unclear is how PME causes this improvement, or whether there’s any cause and effect at all.
“The evidence available so far seems to point to good results,” said conference presenter Eva Lendaro, who’s collaborating with Catalán on PME research. “However, we cannot really at this stage what the mechanisms are. There might be some placebo effect. There also might be some regression to the mean. We need to understand how much [of the improvement] is truly the effect of PME.”
Testing phantom motor execution in a clinical trial
Last year Lendaro directed the first randomized clinical trial of PME. The study involved more than 10 institutions worldwide, including one US partner (the Shirley Ryan AbilityLab). Test subjects were guided through 15 weeks of PME training, while a control group engaged in a basic set of limb exercises that didn’t include PME’s virtual reality and augmented reality features. Subjects from both groups reported their levels of phantom limb pain every week. The core measurement was the reduction in phantom limb pain level from week 1 through week 15.
The test subjects reported immediate improvement, averaging a 33 percent reduction in pain after just one week of PME. By week 7 their average pain reduction improved to 50 percent. At that point it leveled off—after a few ups and downs, the average pain reduction settled back at 50 percent in week 15.
That’s far from a full cure for PLP, but it’s a significant improvement in overall well-being. However, the good news is tempered by the fact that outcomes in the PME test group were only marginally better than the outcomes in the control group. The latter reported a roughly 20 percent reduction in pain after week 1 and a 40 percent reduction after the full 15 weeks. The 10 percent difference in pain reduction between the test group and the control group didn’t rise to the level of statistical significance, so the study failed to confirm the efficacy of PME.
Still, it would be inaccurate to characterize the exercise as a failure. “Pain reduction in the PME group reaches the threshold of 50 percent reduction required for being considered clinically meaningful,” Lendaro says. Future studies, perhaps augmented by brain-mapping MRI imagery or other enhancements, may yet establish a causal link between PME and control of phantom limb pain. Given Catalán’s track record, we’re betting we haven’t heard the last of phantom motor execution.