Skin covers approximately 22 square feet of the human body and accounts for approximately 16 percent of a person’s body weight. It’s our body’s first defense system. When functioning correctly, it protects us from harmful organisms capable of creating intense discomfort or even death.
If you were blessed with “good” skin (amputee lingo for skin that is durable, not particularly prone to irritation, and heals quickly), then bouts of discomfort may be sporadic provided you are dedicated to proper residual-limb skin care; but if you have skin that is prone to rashes, itching, and infection, you have a problem.
If you are a new amputee, preventive skin care of your residual limb begins soon after surgery, and prevention is the key factor in averting complications that result from compromised skin. If you have diabetes with impaired sensation, you should incorporate a thorough visual inspection into your daily routine. Proper cleaning, regular dressing changes, and vigilant monitoring for redness and swelling along the suture lines are important exercises for the prevention of primary infection. In the absence of infection, healing may be relatively quick and can expedite the preparatory phase for your first artificial limb cast.
Lower-limb amputees who use a prosthesis and regularly bear weight on their residual limb may experience skin issues related directly to socket fit. Circulatory pressure or socket rub caused by a socket that is too loose or too tight combined with a humid environment can present mobility challenges. When these conditions are accompanied by pain and lesions, you may need to stop wearing the prosthesis for a period of time for healing to occur.
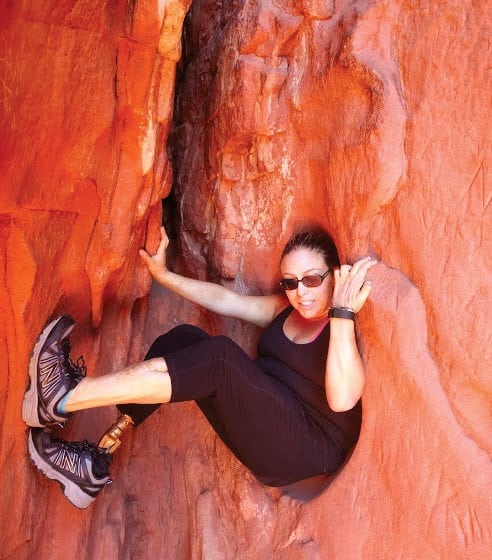
For Olivia Leigh, from Denver, skin issues and repeated interruptions of her mobility not only affect her physical health, but her emotional health as well. Since losing her leg in 1999 due to a terrorist bombing, Leigh’s right, below-knee traumatic amputation has been a constant source of anger and frustration. During the first ten to 12 years, cysts frequently interfered with her ambulation.
“Doing anything was difficult,” says Leigh. “Even being nonambulatory, the cyst would swell without the pressure of my prosthesis, and moving [my leg] would be so painful. Getting up to go to the bathroom or crawl anywhere was extremely painful. I was going to school, working, and trying to live life and always preferred to have my leg on, even if it was painful, so life was exhausting and draining. I’d have to carefully consider anything I needed to do. It was a gut-wrenching cycle.” Keeping the skin on Leigh’s residual limb in check now involves consistently cleaning her liner every night, using A+D Cream on scar tissue and cyst-prone areas, and making sure her prosthesis is fitting properly.
Timothy R. Dillingham, MD, MS, physiatrist in chief, Penn Medicine, University of Pennsylvania, emphasizes that regular prosthetic liner maintenance, keeping skin that is in contact with the liner dry and clean, and maintaining proper socket fit and alignment are all vital to a safe and highly functional outcome for amputees at all levels.
“Most of what I see are [skin issues] due to a socket that is not fitting well,” says Dillingham. “Ingrown hairs can occur at the margins of the socket due to excess pressures. Small skin cysts and overt skin breakdown can occur in these areas of chronic compression or shear stress. Sometimes small fluid-filled sacs, or bursae, develop under areas of excess socket pressure.
“Other things I see,” continues Dillingham, “are people who have a hard socket that is too large. Consequently, they add socks, which then prevent them from getting fully down into the socket. This process can lead to dependent edema in the end of the limb. Over time, chronic edema can progress to a wart-like skin condition called verrucous hyperplasia. The treatment for this is to have a socket that provides total contact and will provide pressure over the distal end of the limb.”

Fungal infections similar to athlete’s foot are also common. “Contact dermatitis can be seen. It’s skin–so anything you can get on your foot or other parts of your skin can happen on your residual limb as well,” says Dillingham. Confirmation and treatment may involve a consultation with a dermatologist.
It’s important that amputees not overlook even the slightest irritation of the skin beneath their liner. The warm and humid environment surrounding the limb provides the perfect breeding ground for bacteria. Even a pimple can mean trouble, as Diane Wales, from Aurora, Colorado, found out. Despite a course of antibiotics, it wasn’t until Wales took an airline flight that things became serious quickly. Because Wales was unaware that amputees using a vacuum prosthesis should remove it during flight, the once-tiny pimple ballooned to an open wound one-third of an inch in diameter.
Following three rounds of different antibiotics, the sore continued to enlarge. After five-and-a-half months of collagen and small intestine submucosa (SIS) therapy at a wound clinic, the wound eventually granulated and healed; however, Wales was unable to work for six months, resulting in termination from her position as a labor and delivery nurse. The chain reaction of events left her emotionally and financially drained.
“I am very faithful about handling my residual limb with clean hands and wash my liner every night when I take it off,” she says. “If I get any sort of a bump or pimple on my limb, I now use a topical application of mupirocin ointment on the spot until it clears up, and I give my limb more out-of-socket time when able. I will never again ignore a bump on my limb….” — By Elizabeth Bokfi
Most of what I see are [skin issues] due to a socket that is not fitting well. — Timothy R. Dillingham, MD, MS

Ideas for Dealing With Common Issues
Following are several general ideas for preventing and dealing with skin problems. While they have worked for some amputees, there is no guarantee that they will work for you. It is important, especially if you have diabetes or a vascular disorder, to discuss your condition with a qualified healthcare professional and find the right solution for you.
Skin Breakdown
Although characteristics of skin breakdown vary, the first stage may be felt as a sudden burning sensation, sometimes behind the knee or at the elbow crease.
Potential solutions include:
- Cutting away the excess fabric of your prosthetic sock near the top of your socket to reduce bunching, which is often a cause of breakdown
- Cleaning your limb with a fragrance-free cleanser and towel drying it completely before donning your prosthesis
- Using an antiperspirant mist prior to donning your silicone sleeve to reduce the amount of sweat generated in your liner; the salt in sweat can cause itching, and the sweat itself soaks the skin, increasing the chances of breakdown
- Removing, washing, and drying your prosthetic liner after physical activity
Pulling
During ambulation, the silicone liner grips and pulls the skin.
Potential solutions include:
- Applying a viscous ointment over areas that have callused to relieve pulling
- Paying special attention to scarred areas; even well-healed sutures can develop into problem areas years after surgery
Bottoming Out
Amputees who bear weight on their prosthesis may experience problems when strenuous activity or rapid atrophy results in bottoming out at the distal end of their socket, indicating that it has become loose-fitting. Pain and bruising may be present.
Potential solutions include:
- Adding an extra sock or two to lift the limb slightly and relieve the pressure on its end
- Having your prosthetist add an adjustment fill at the patellar shelf if you are a below-knee amputee
- Removing the prosthesis temporarily to facilitate healing if blisters have occurred
Choking
Reduced blood flow, referred to as choking, is often the result of the socket or liner being too tight. The limb may appear red or bluish black, and if left untreated, choking can lead to tissue necrosis.
Potential solutions include:
- Having your prosthetist grind out certain areas inside your socket to provide relief
- Rolling your liner onto your limb slowly and carefully to ensure complete contact with your skin’s surface and prevent pinching the skin
- Rolling a new liner over the end of a large soda pop bottle to stretch the liner
Pressure Points
These are small localized areas of pressure that can result in abrasions, blisters, calluses, and skin breakdown. Complications may include infection from the skin being broken and exposed to bacteria. Pressure points can change from day to day or even hour to hour, depending on volume changes due to weather and your activity level.
Potential solutions include:
- Monitoring common pressure points, such as those on both sides of your knee and the distal end of your residual limb for skin breakdown; cutting a hole in your prosthetic sock can be a temporary fix when you’re out and about
- Having your prosthetist cut away a portion of your socket to relieve pressure