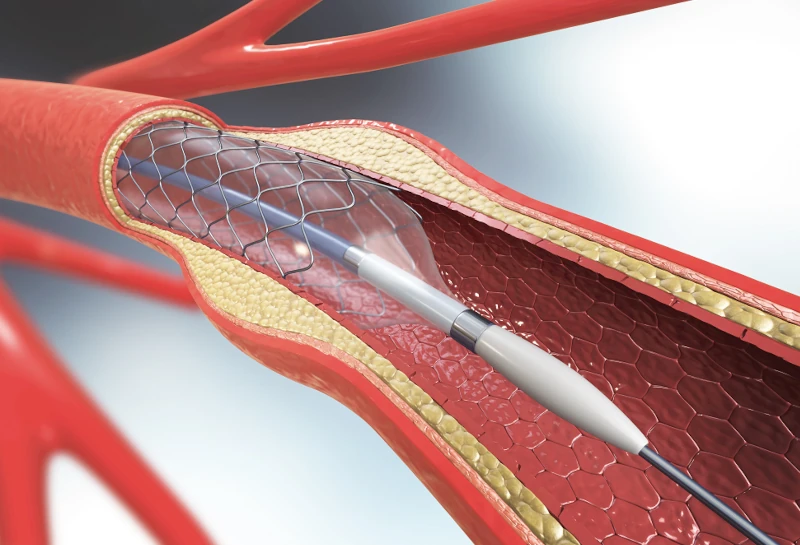
Surgeons routinely use artherectomies, vascular implants, and other interventions to improve leg circulation and preserve limbs that are at risk of being lost. But when these procedures are abused for profit, they can end up hastening amputation rather than preventing it.
That’s the unfortunate conclusion reached by investigative reporters at the New York Times and ProPublica. Both outlets have published articles this year documenting the growing incidence of amputation caused by misguided overuse of revascularization treatments. The Times article, which appeared just a few days ago in the Sunday edition, focused on artherectomies, in which doctors thread an instrument into clogged arteries and scrape deposits from the vessel walls to promote better blood flow. ProPublica’s report, which appeared in February, spotlighted the overzealous use of vascular inserts (stents and balloons) to widen blood vessels.
When used appropriately, these are legitimate treatments that can indeed prevent limbs from being lost. But when they’re performed on patients who have mild or no symptoms, the interventions can (and often do) lead to amputations that might otherwise have been unnecessary.
Why are some doctors prescribing so many of these procedures on patients who don’t really need them? Take a wild guess.
“There is a clear business motive for treating people with no symptoms,” said Johns Hopkins surgeon Caitlin Hicks in a statement to the Times. Hicks authored a peer-reviewed scientific study that concluded: “There is a critical need for professional guidelines outlining the appropriate use of atherectomy in order to prevent overutilization of this technology, particularly in high-reimbursement settings.” Hicks told ProPublica: “Atherectomy is important in certain settings. But it’s being used in a way that is entirely inappropriate, and it’s largely driven by the incentive structure.”
The Times backed up that conclusion by showing that the number of artherectomies performed each year has more than doubled since 2011, when Medicare started offering generous reimbursement for outpatient artherectomies. Annual Medicare payments for artherectomies leapt from $86 million to $612 million during the same period, and the number of outpatient clinics devoted to PAD mushroomed from near zero to more than 800. The Times also found that the doctors who perform the highest volume of artherectomies routinely have financial relationships (including loans, research sponsorships, and consulting gigs) with corporations who manufacture medical devices that are used in these procedures.
The Times report names names, citing Michigan surgeon Jihad Mustapha, Texas practitioner Ralph Brookshire, and Pennsylvania radiologist James McGuckin as particularly egregious abusers of the system. All three have been investigated by medical regulators and/or sued by the federal government.
ProPublica’s article centered on a whistleblower suit alleging that medical pros at a Kansas VA hospital got illegal kickbacks from the medical device manufacturer Medtronic, as rewards for high-volume deployment of the company’s vascular implants. The article documented one case in which a Medtronic sales rep actually attended a vascular procedure and texted a running tally of the number of devices (each one costing thousands of dollars) implanted into the patient. That particular individual ended up with nearly 20 Medtronic stents and balloons in their body. In another case, the surgeon deployed 33 devices during a single procedure.
According to documents filed as a part of the whistleblower suit, the VA’s own experts determined that its doctors routinely pursued overaggressive treatment for PAD, failed to follow evidence-based medicine, disregarded established best practices for treatment, and overused drug-coated balloons and artherectomy devices. At the same time, the number of amputations performed at the hospital increased sixfold.
The growing outcry against this trend isn’t only coming from patients who’ve suffered bad outcomes. Doctors and medical ethicists are joining the chorus. “Someone who cuts or inserts something into a patient for unnecessary work is the same as someone stabbing you in the street and taking your wallet,” one vascular surgeon told the Times. And researchers at Dartmouth published data which showed that “atherectomy is used to treat peripheral arterial disease, even though long‐term adverse outcomes occur more frequently after this treatment modality. . . . . The inferior outcomes and higher cost of atherectomy relative to other treatment options calls into question the ubiquitous use of atherectomy in clinical practice.”
If you’ve lost a limb due to what you consider aggressive use of artherectomy, vascular implant, or other revascularization procedures, contact us at editor@livingwithamplitude.com.