When it emerged in the early 2000s, targeted muscle reinnervation (TMR) was hailed as a game-changing surgery for upper-limb amputees. By enabling powerful new connections between the nervous system and the prosthesis, TMR opened the door to a generation of groundbreaking bionic devices.
Now a consensus is forming around TMR’s potential benefits for a larger class of patients: leg amputees, including those with concurrent health challenges.
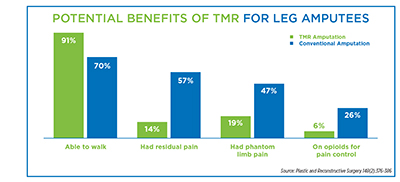
A recent study of roughly 200 below-knee amputees showed that primary TMR (which is performed at the time of amputation) dramatically reduces phantom limb pain, post-operative neuromas, and opioid dependence, while increasing patients’ mobility and overall fitness. Conducted at the Georgetown University School of Medicine and published in the medical journal Plastic and Reconstructive Surgery, the study focused on individuals who generally struggle to achieve good post-amputation outcomes: older patients with comorbidities such as diabetes, vascular disease, obesity, and kidney disease.
Such health complications routinely impede new leg amputees’ ability to resume walking. Yet 91 percent of the patients in the Georgetown study were ambulatory nine months after amputation. Only 19 percent experienced phantom limb pain, and just 6 percent were taking opioids for pain control. All of these outcomes represent dramatic improvements in quality of life, while auguring better long-term health and life expectancy.
Building on the Georgetown study, a team of doctors at Yale University estimated that TMR could benefit as many as 40,000 new amputees every year. In a forthcoming paper accepted for publication in Orthoplastic Surgery, they argue that “a significant proportion of amputee patients may be eligible for TMR who may not previously have been considered candidates for the procedure.” This segment includes individuals with diabetes, hypertension, and vascular disease, all of which run rampant within the amputee population. “TMR is becoming an important treatment option for patients with significant comorbidities including peripheral vascular disease, as well as older patients,” the Yale doctors conclude.
Although both the Yale and Georgetown studies focus on primary TMR, there’s promising data on the benefits of secondary TMR, in which the surgery is performed months or years after limb loss. The most significant research of this type, a randomized controlled trial written up in Annals of Surgery in 2019, found that secondary TMR substantially reduced phantom limb pain. However, that patient cohort was younger and healthier than the population in the Georgetown study. It remains to be seen how much secondary TMR would improve quality of life for older amputees with serious health challenges.
The trajectory remains promising nonetheless, and the Yale study’s bottom line rings true: “The availability of TMR should be widely expanded.”



